Lesson of the Week

To be at peace means giving up the need to control everything. Anyone else get klunked on the head with a life lesson, recently?

To be at peace means giving up the need to control everything. Anyone else get klunked on the head with a life lesson, recently?


Caregiving is filled with difficult discussions and End-of-Life talks are particularly hard, uncomfortable, and can even feel insensitive, at times. The key, though, lies in reframing these conversations as acts of love that satisfy a dual need for both you and the person you’re caring for. Not only does your parent/grandparent/spouse/partner have the right to be heard and respected for their choices, but this kind of validation can also bring them comfort and piece of mind. This is the very same thing it can do for you as it removes the burden of trying to guess what their wishes are in a time of crisis.
A good place to begin is with talking to your adult family member about the kind of medical care they want and don’t want as they grow older, become ill, or if a catastrophic health event were to occur. Some questions might focus on their priorities such as wanting comfort care over aggressive treatments; preferring hospice care at home, if possible, over spending final days in a hospital; or embracing quality of life over quantity.
These conversations are deeply rooted in a person’s values, beliefs and what is most important to them, and even if your family member is in the early stages of a dementia diagnosis, he or she may still have a strong desire to make their preferences known.
Talking about it isn’t enough, though. Their wishes must be outlined in a legal document called a Living Will, also known as an Advance Directive. The Advanced Directive spells out instructions regarding preferred medical care if a person is unable to communicate this information on their own.
There’s another necessary legal document that names a Healthcare Surrogate, aka Healthcare Proxy, or Healthcare Power of Attorney. This person becomes the voice of the patient if they’re unable to speak, so this needs to be someone who the patient trusts to do their best in terms of ensuring that medical personnel carry out their wishes. It’s a hugely important role, and one that not just anyone can fulfill. In fact, when I was going down the list of potential prospects for me personally, I ended up choosing my ex-husband, who I will say, was very enthusiastic – almost too much so!
Finally, another critical health-related document to discuss early on is the Do Not Resuscitate form, or DNR, a formal doctor’s order that must be completed and signed by a physician and your family member. Essentially, it states that CPR should not be performed if they stop breathing or their heart stops beating.
The reason this form is so critical has to do with the effectiveness of CPR procedures, which include mouth-to-mouth resuscitation, but also electric shock, inserting a tube into a patient’s airway, and even open-chest heart massage. If someone is already in a fragile state, CPR may leave him or her in profoundly worse condition than before. It’s a very personal choice but one that needs to be made ahead of time. For the record, during the time I helped care for my mom, I carried this document with me in my Caregiver Purse, and always made a point of letting hospital personnel know about it. Sometimes, I felt like the Angel of Doom, but making sure my mother’s wishes were honored was always what guided me.
So what should happen next? Make copies like crazy and share t with all healthcare personnel involved in your family member’s care. Keep a set in the person’s home. If they live in a residential care community, make sure the administration has the documents, and always keep copies that you can put your hands on quickly. Also, give to the hospital and/or ER whenever your loved one is admitted. Don’t assume that if you gave it to them once, it will be enough. With the DNR in particular, make sure it’s in a place that can be clearly seen in your family member’s home or room.
Two good websites for more guidance on Living Wills include: AgingWithDignity.org, which offers a form called 5 Wishes, a type of Living Will that addresses emotional, spiritual, and personal needs in addition to the medical side of things. The other site is TheConversationProject.org, which actually offers conversation-starter kits to help individuals and families feel more comfortable when talking about end-of-life choices.
There is nothing easy about having these kinds of talks, which can often be very emotional experiences. And it’s ok to say that it makes you uncomfortable, and you’re unsure how to begin. But, as a family caregiver, having the courage to take the lead on this can actually offer an opportunity to create an even deeper relationship with the person you’re caring for. Who wouldn’t want that?
Note: Another important conversation has to do with seeking a loved one’s input regarding their funeral or memorial service. Again, it may seem like a subject you shouldn’t bring up, but in reality it’s a way of showing your respect by wanting to honor their final wishes. For more info, see this post (a reader favorite) about planning my mom’s funeral with Barbra Streisand’s help.
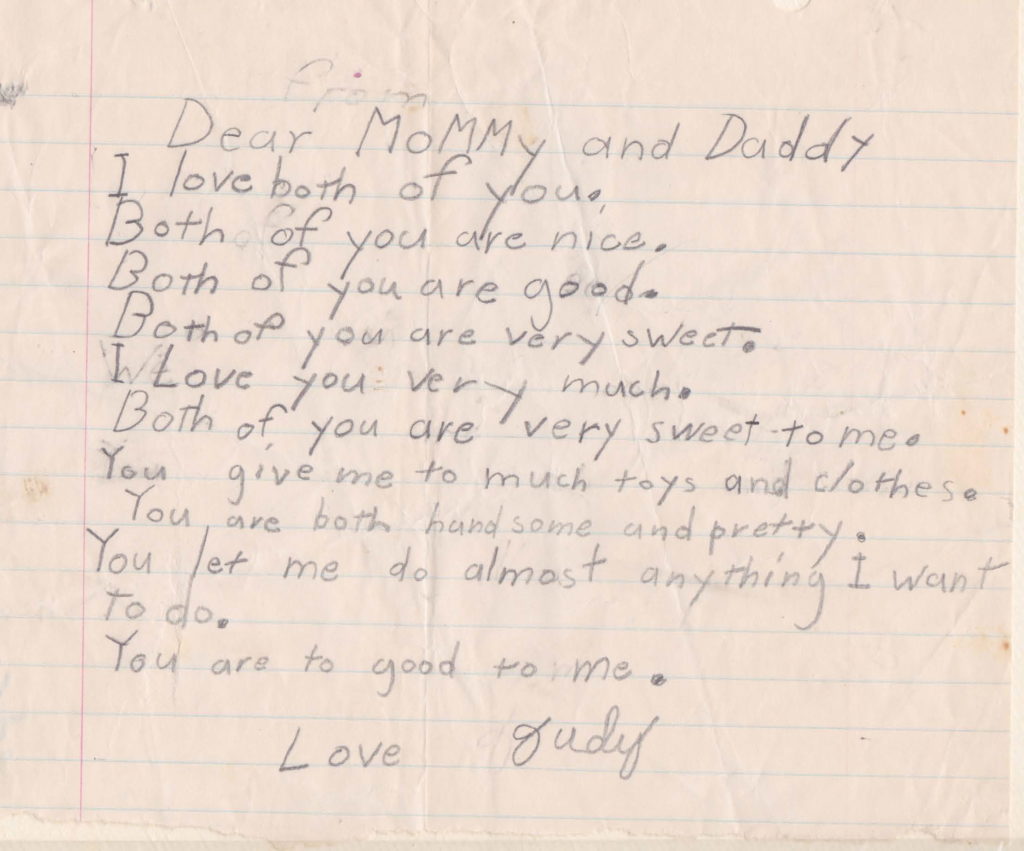
A moment from the past. Is it any wonder that caring for my parents in their later years, and writing a book about it, was the natural thing to do? Many thanks to the Florida School System for eventually teaching me the difference between “to,” “too,” and “two.”

You can take the girl out of caregiving, but you can’t take caregiving out of the girl. Right now, there are nine different herbs planted in pots on my back porch. They have names like Rosy, Cilia, and Dilly – all decidedly female, even Reggie One and Reggie Two, the oreganos. I talk to these gal pals throughout the day, giving them reassuring little leaf rubs, keeping them hydrated, looking out for leaf blight, and offering lots of reassurance. This, of course, could be considered either crazy or endearing, depending on whether you embrace a bit of woo-woo in your life. The thing is, they look like they’re smiling, and that delights me. This, coming from the person who, years ago, told new plants, “I hope you stick around, but there are plenty more where you came from.”
Digging deeper, I’m figuring out this goodness stems from being open to embracing new ideas and practices that inspire and sustain me. Exactly what I want for YOU, beginning with this essential truth. Whether currently a caregiver or a perennial – you, me, and the thriving plants on my deck have something in common. Like them, we can grow. We can bloom. We can flourish. What it takes is our encouragement, our attention, and our kindness to each other.
————–
What or who inspires you?
Is there a creative activity you’d like to try out, or get back into?
What is your favorite thing to do when you have a little time?
(If it’s “sleep,” I suspect you’re in caregiver mode.)